Ziehl Neelsen Stain Of Bronchial Washing
The Ziehl-Neelsen stain is a critical diagnostic tool in microbiology, particularly for detecting acid-fast bacteria in clinical samples. When applied to bronchial washing specimens, this staining technique allows pathologists and microbiologists to identify pathogens such as Mycobacterium tuberculosis, which are responsible for severe respiratory infections. Bronchial washing, a procedure performed during bronchoscopy, involves rinsing the bronchi with sterile saline to collect cellular material and microorganisms from the lower respiratory tract. The combination of Ziehl-Neelsen staining with bronchial washings provides a highly sensitive method for diagnosing pulmonary tuberculosis and other infections caused by acid-fast organisms, offering rapid and reliable results compared to traditional culture methods.
Understanding Ziehl-Neelsen Staining
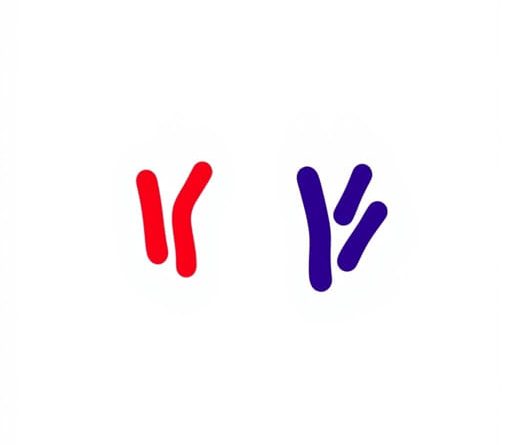
The Ziehl-Neelsen stain, also known as the acid-fast stain, was developed in the late 19th century by Franz Ziehl and Friedrich Neelsen. It is specifically designed to detect acid-fast bacteria, which possess a unique cell wall rich in mycolic acids. These lipids make the bacterial cell wall resistant to decolorization by acids during the staining process, allowing these organisms to retain the primary stain, carbol fuchsin, even after treatment with acid-alcohol solutions. The acid-fast nature of these bacteria distinguishes them from non-acid-fast organisms, which readily lose the stain and take up a counterstain such as methylene blue.
Principle of the Staining Method
The principle of Ziehl-Neelsen staining is based on the affinity of mycolic acids for lipid-soluble dyes. Carbol fuchsin penetrates the waxy cell wall when heat is applied, binding to the lipids within. After staining, the slide is treated with an acid-alcohol solution, which decolorizes non-acid-fast cells while the acid-fast bacteria retain the red color of carbol fuchsin. Finally, a counterstain such as methylene blue is applied to provide contrast, allowing the background cells to be seen clearly under the microscope. This differential staining technique makes it possible to identify acid-fast bacteria even in complex clinical specimens like bronchial washings.
Bronchial Washing Sample Collection
Bronchial washing is performed during bronchoscopy, a procedure where a flexible tube with a camera is inserted into the airways to visualize the bronchi and collect samples. Sterile saline is instilled into specific areas of the bronchial tree and then suctioned back, carrying with it cells, mucus, and microorganisms. The collected bronchial wash fluid is then prepared on slides for staining or sent for microbiological culture and molecular testing. Bronchial washings are especially useful in patients who are unable to produce sputum or have negative sputum smears, providing an alternative route to obtain lower respiratory tract specimens for diagnostic testing.
Advantages of Using Bronchial Washings
- Improved sensitivity for detecting pulmonary pathogens, particularly in smear-negative cases.
- Ability to sample specific regions of the lungs, enhancing targeted diagnosis.
- Collection of both cellular and microbial material for comprehensive analysis.
- Reduced contamination with oral flora compared to expectorated sputum.
Performing the Ziehl-Neelsen Stain on Bronchial Washings
Once the bronchial washing specimen is collected, it is concentrated by centrifugation to obtain a pellet containing cells and microorganisms. A smear is prepared from the pellet, air-dried, and heat-fixed onto a glass slide. Carbol fuchsin is then applied to the smear, typically with gentle heating to enhance dye penetration. After staining, the slide is rinsed and treated with acid-alcohol to remove the dye from non-acid-fast cells. A counterstain, usually methylene blue, is applied to provide a contrasting background. The slide is then examined under oil immersion microscopy. Acid-fast bacteria, including Mycobacterium species, appear bright red against a blue background, allowing for clear identification.
Interpretation of Results
Microscopically, the presence of bright red rods against a blue background indicates acid-fast bacteria. The quantity and morphology of the stained organisms can provide information about the bacterial load and species. Ziehl-Neelsen staining is qualitative and semi-quantitative, offering immediate visual confirmation of infection, which is particularly valuable in diagnosing tuberculosis. Negative staining does not completely rule out infection, so Ziehl-Neelsen results are often supplemented with culture or molecular techniques for definitive identification.
Clinical Significance
The Ziehl-Neelsen stain of bronchial washings is particularly important in the diagnosis of pulmonary tuberculosis, especially in patients with negative sputum smears or atypical clinical presentations. Early detection of acid-fast bacilli allows for prompt initiation of anti-tubercular therapy, reducing the risk of disease progression and transmission. Beyond tuberculosis, the technique can also detect other acid-fast organisms such as Mycobacterium avium complex, aiding in the diagnosis of opportunistic infections in immunocompromised patients, including those with HIV/AIDS.
Limitations and Considerations
- Ziehl-Neelsen staining is less sensitive than culture or nucleic acid amplification tests for low bacterial loads.
- Proper technique is critical; inadequate heat application or over-decolorization can lead to false negatives.
- Bronchial washing samples may contain debris that can obscure microscopic examination.
- Complementary diagnostic methods are often required to confirm species identification.
Advancements and Complementary Methods
Modern diagnostic laboratories often combine Ziehl-Neelsen staining with molecular techniques, such as polymerase chain reaction (PCR), to enhance sensitivity and specificity. Automated staining systems and fluorescence-based acid-fast staining methods, such as auramine-rhodamine staining, offer faster results and easier detection under fluorescence microscopy. Nevertheless, the Ziehl-Neelsen stain remains a cost-effective, widely used, and reliable method in resource-limited settings for detecting acid-fast bacteria in bronchial washings and other clinical specimens.
The Ziehl-Neelsen stain of bronchial washing samples is an essential procedure in clinical microbiology, providing rapid and effective detection of acid-fast bacteria such as Mycobacterium tuberculosis. By leveraging the unique properties of the acid-fast cell wall and combining careful specimen collection via bronchial washing, this technique enables healthcare professionals to diagnose respiratory infections accurately. Despite its limitations, the Ziehl-Neelsen stain continues to be a cornerstone in tuberculosis diagnosis and monitoring, particularly in areas with high disease prevalence. When complemented with culture and molecular methods, it forms part of a comprehensive diagnostic strategy that can guide timely treatment and improve patient outcomes, highlighting its enduring importance in modern medical practice.